Flexor tendons - General


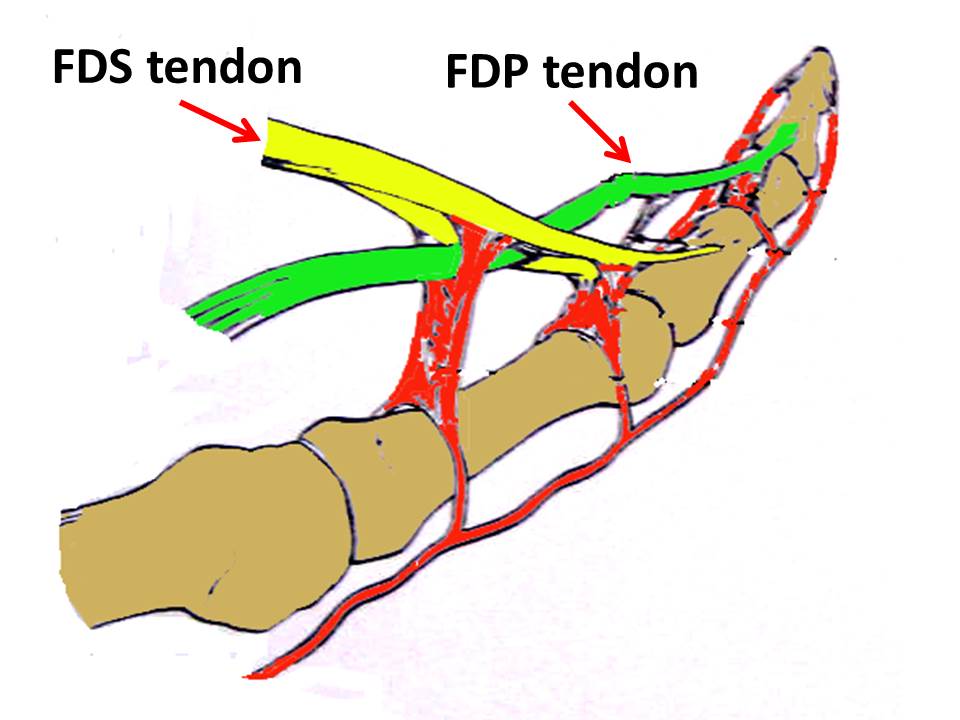
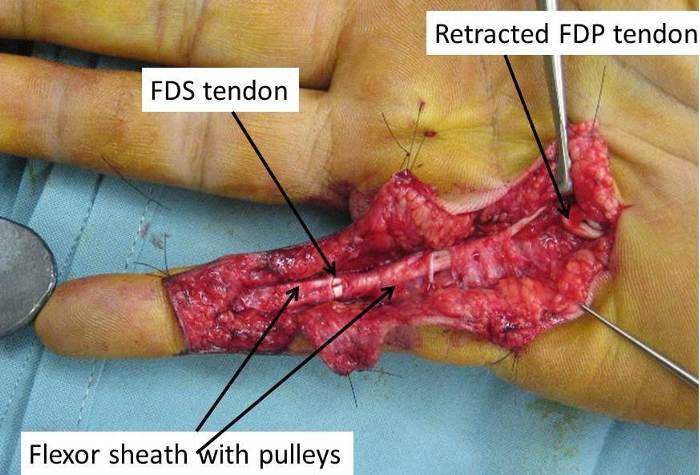
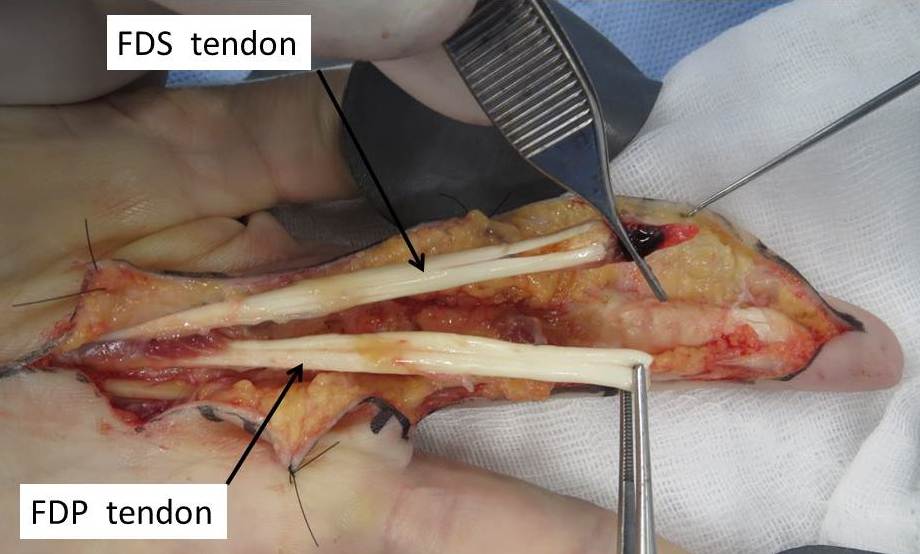
There are 2 tendons acting on each finger to bend or flex the finger.
FDS = Flexor Digitorum Superficialis, ( Superficial tendon) Flexes the PIP joint
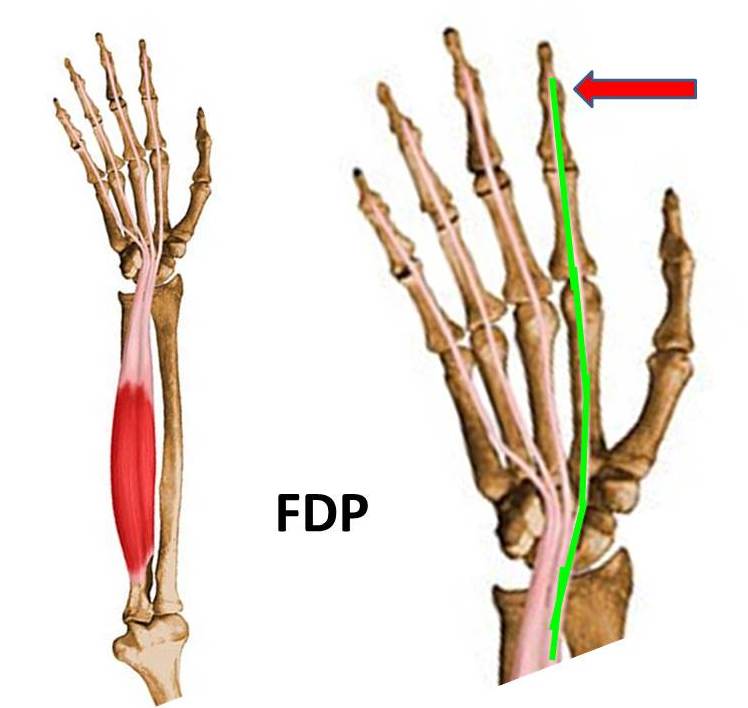
FDP = Flexor Digitorum Profundus ( Deep tendon) Flexors all joints in the finger
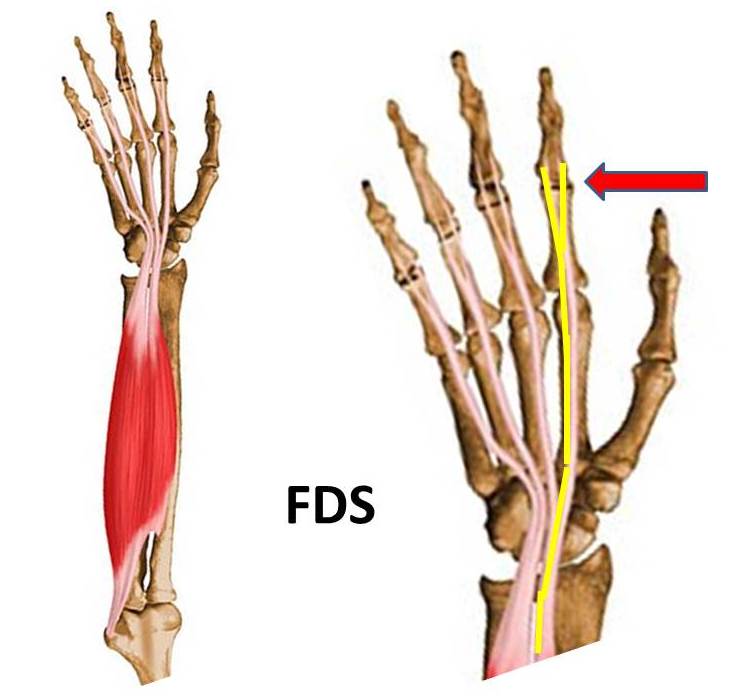
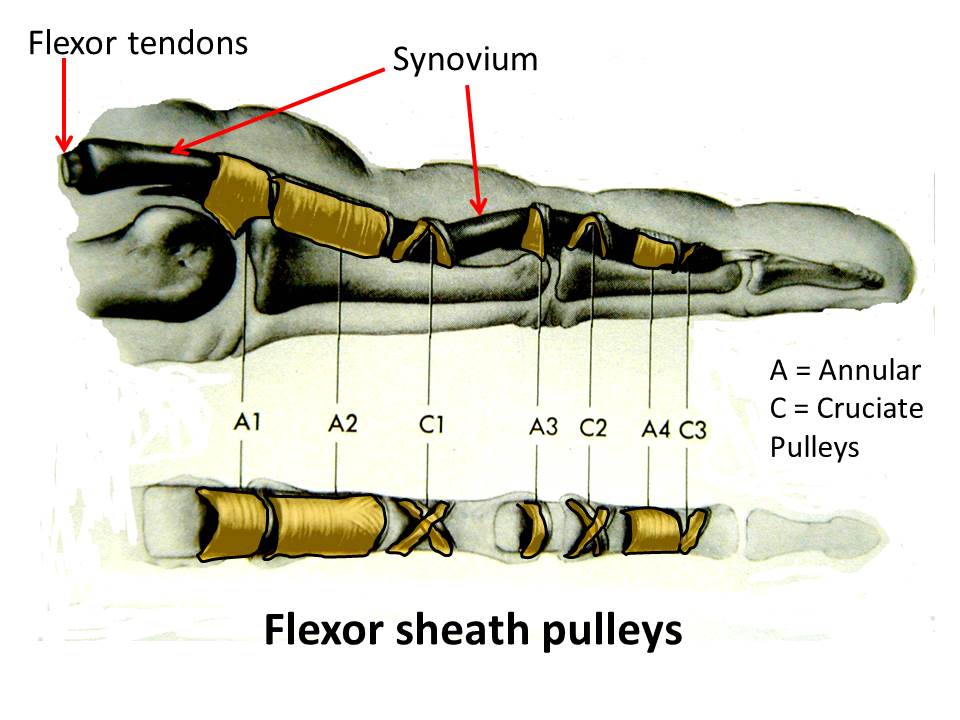
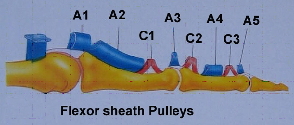
The tendons run up the front of the finger in a tunnel ( Flexor sheath ) which is lined by synovium , a lubricating tissue which allows the tendon to glide without resistance.
Thickenings of the flexor sheath are called pulleys and they hold the tendon down against the bone and prevent bowstringing.
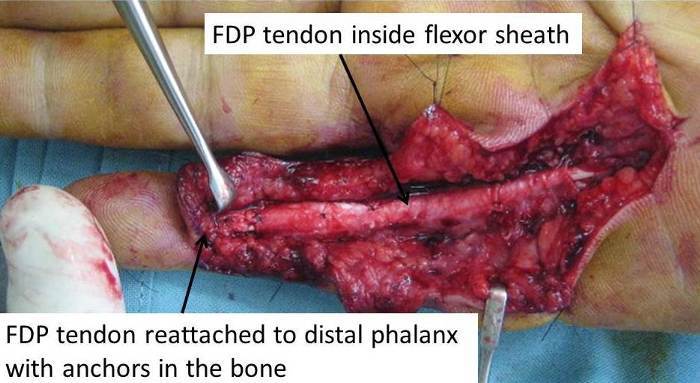
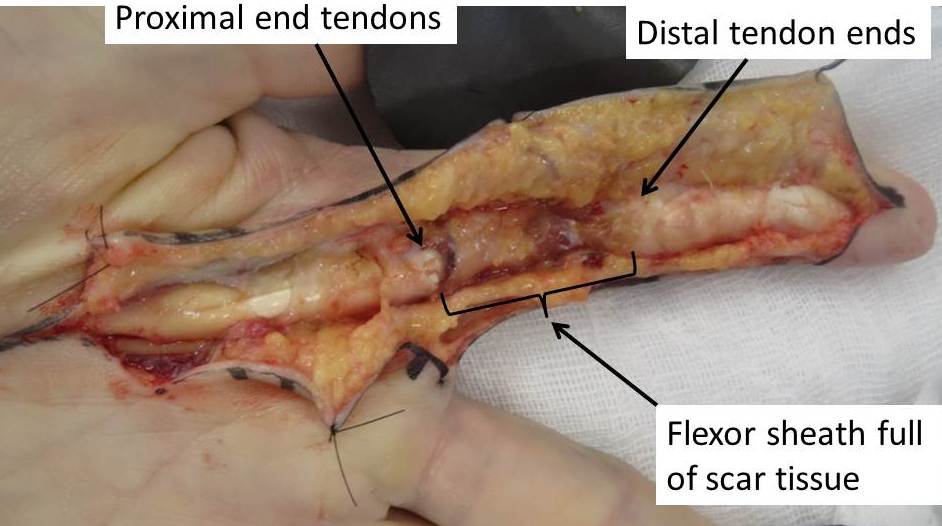
When a tendon is cut or pulls off the bone it results in bleeding up and down the sheath.
The blood turns to scar tissue and hinders normal gliding of the tendons.
Direct repair of a tendon is therefore only possible for 2 – 3 weeks after an injury.
After this time the scaring becomes too dense and the tunnel becomes narrowed and rough thus preventing smooth gliding of the tendon.
The muscle continues to act on the proximal end of the tendon. This muscle effect results in the tendon retracting so that over a period of time the gap between the divided tendon ends becomes great.
POSSIBLE CAUSES:
- Tendon lacerations. May be apparently a minor laceration but can result in division of both flexor tendons.
- Football tackles - finger caught in an opponents jersey ( Hence "Jersey Finger" )

TREATMENT:
1. Direct repair
- Early repair provides the best results. Need to be performed within 2 weeks.
- Laceration wounds may be extended to allow direct suture of tendons or re-attachment to bone ( Jersey finger)

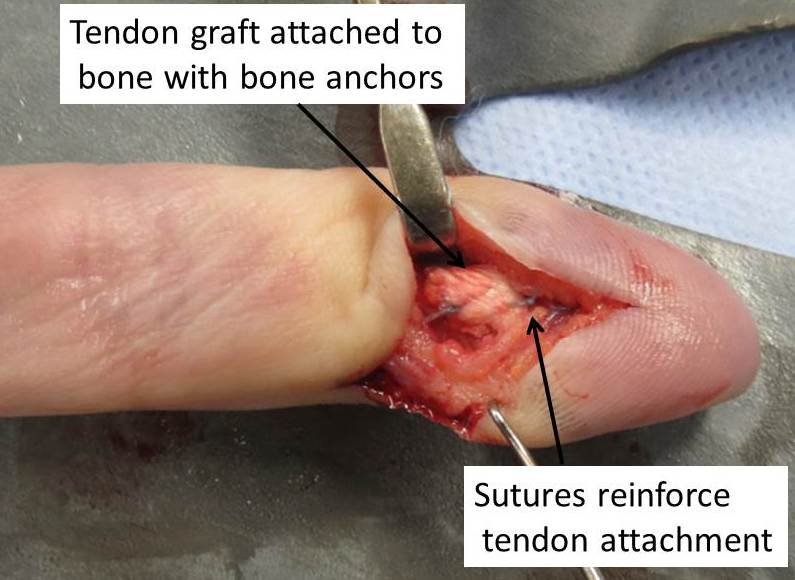
- Tendon reattached using button on back of finger or bone anchor

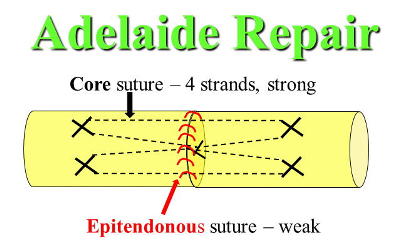
- Sutures complex and designed to provide adequate strength to the repair without being too bulky
- Stay overnight in hospital
- Plastic splint 6 weeks

- Significant activity restriction for 3 - 4 months
- Extensive Hand therapy
Late Presentation - Options in treatment:
1. Do Nothing
- Finger tip unable to bend
- Pain in finger or palm may never completely settle
- May develop carpal tunnel syndrome due to swelling in the palm
- May result in limitation of movement at PIP joint
2. Resect the retracted tendon
– if pain persists in the palm
- May also improve range of motion at PIP joint
3. Fuse the end joint (D.I.P.) of the finger
- Small cut on back of finger
- 6 weeks in a splint
- No significant need for physiotherapy
- Pain in finger or palm may never completely settle
- May develop carpal tunnel syndrome due to swelling in the palm
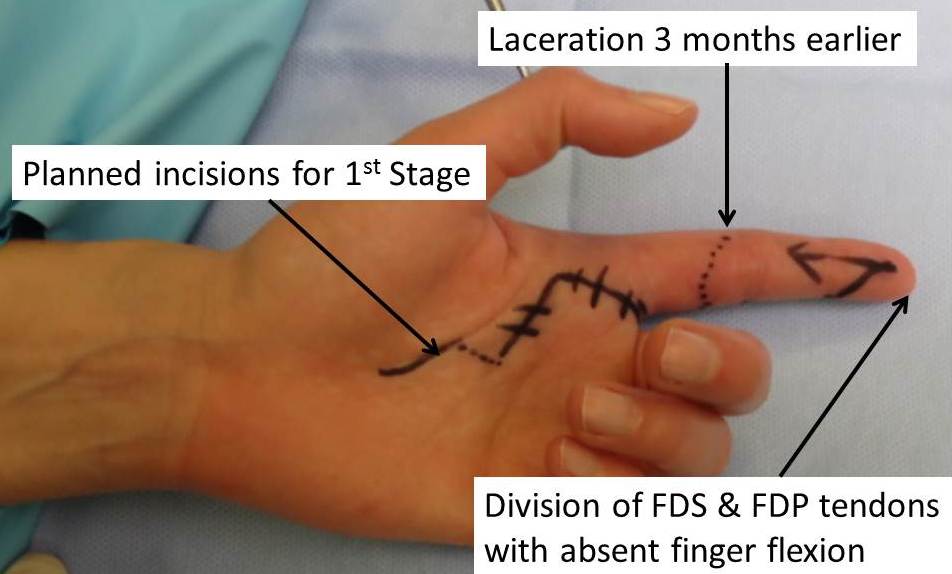
4 . 2 Stage flexor tendon graft
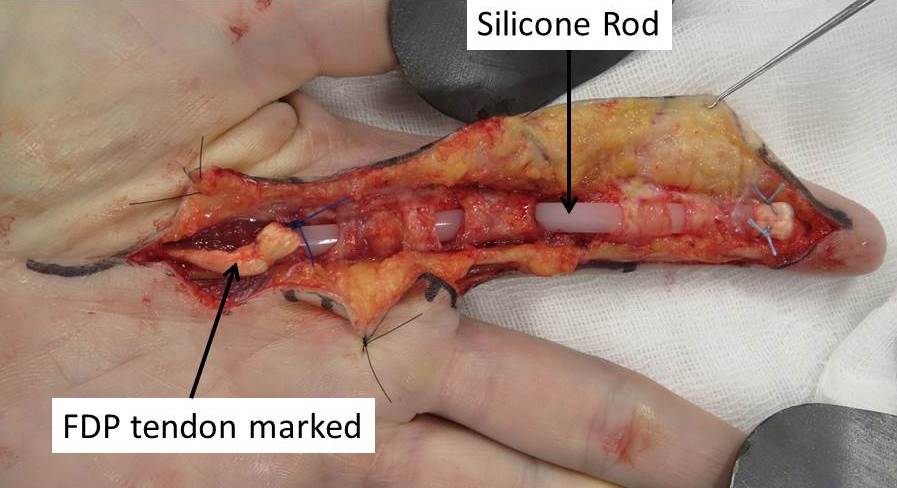
1st Stage
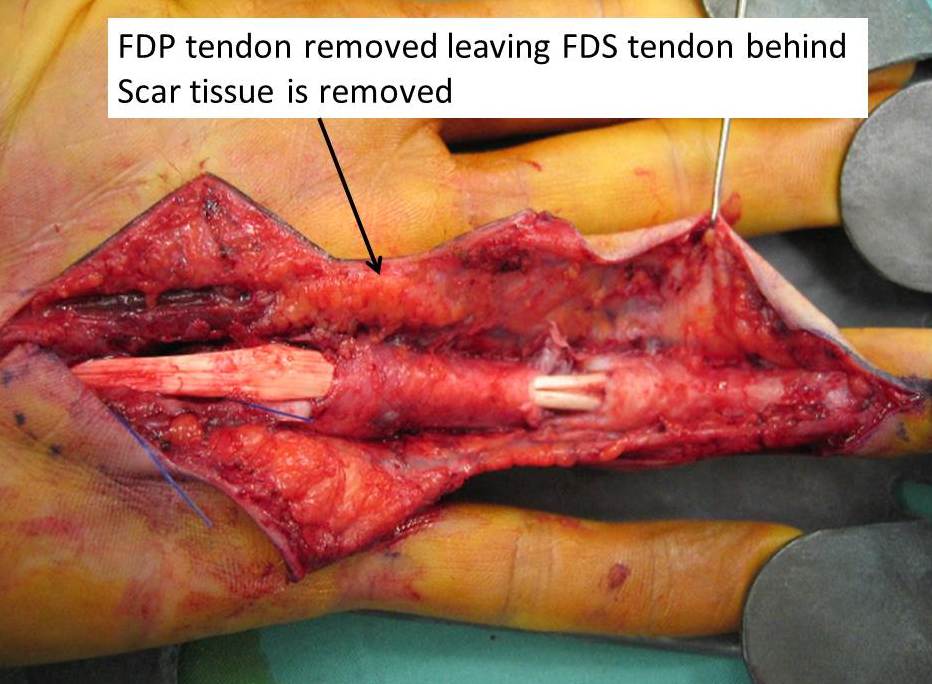
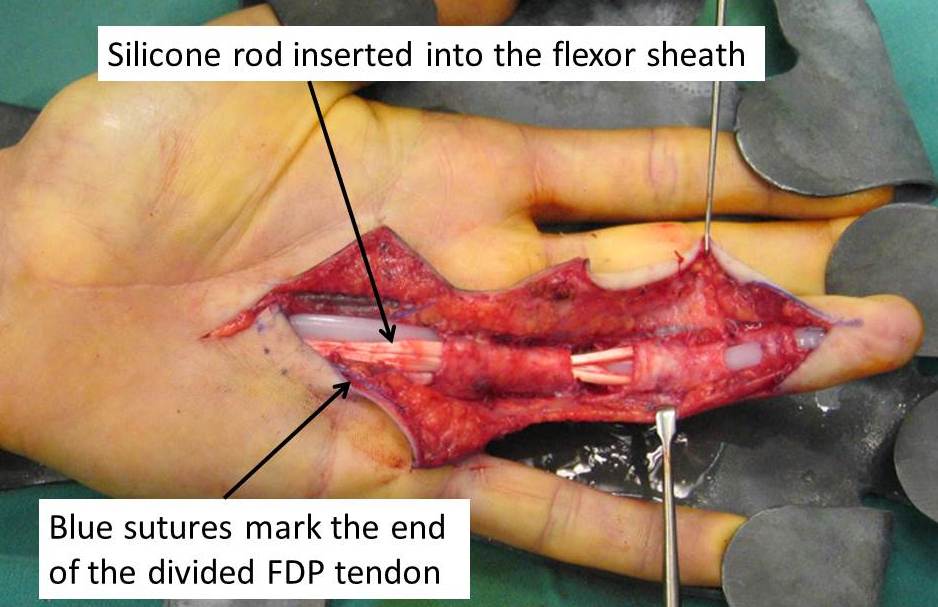
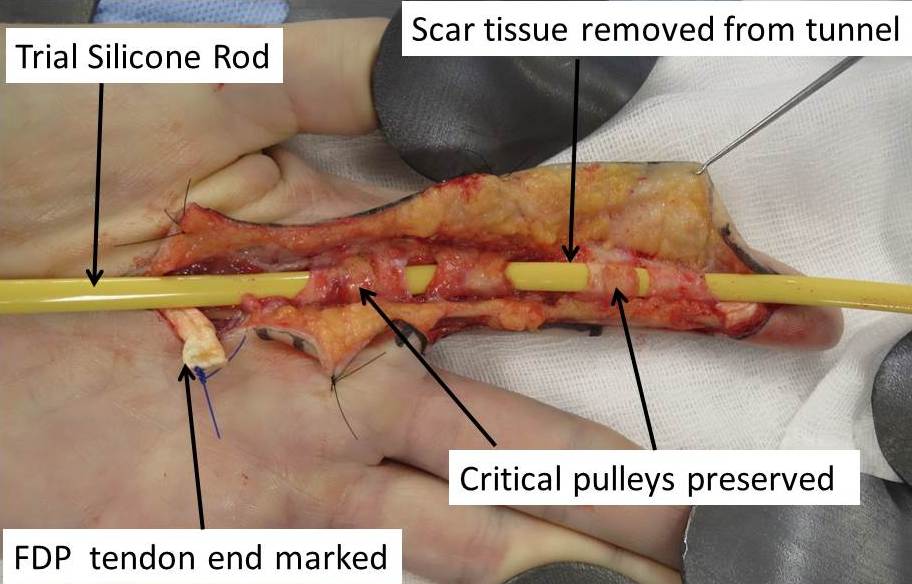
- Extensive incision along finger and in palm to remove the lacerated tendons and scar tissue

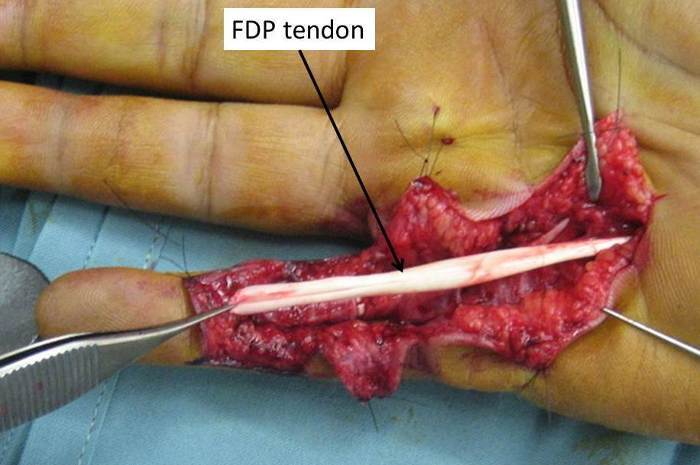
- Insert a Silicone Rod in the tendon sheath.
- Tendon sheath may require reconstruction
- The body reacts to the Silicone - and "walls off" the rod with smooth tissue in essence recreating a smooth tunnel
- Overnight stay in hospital
- Wound heals after 2 weeks
- No splintage
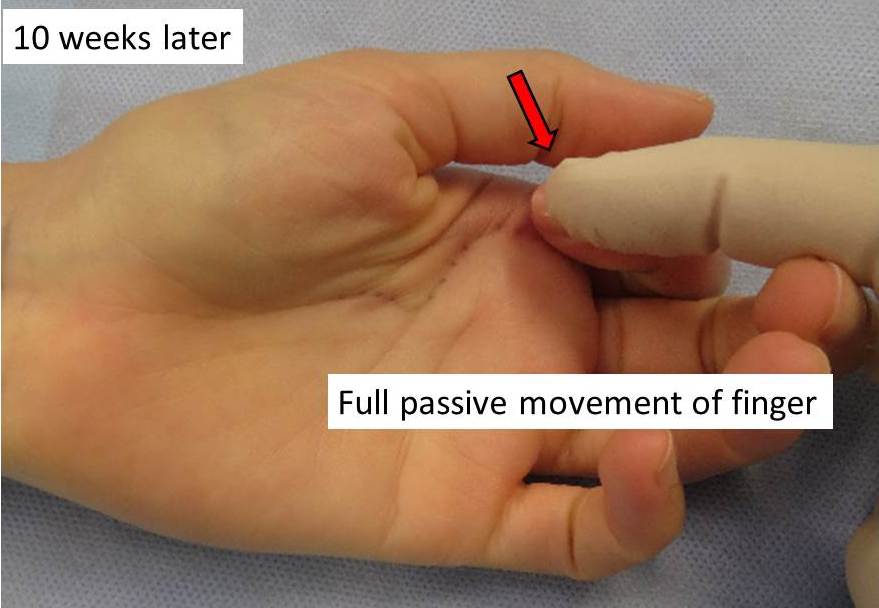
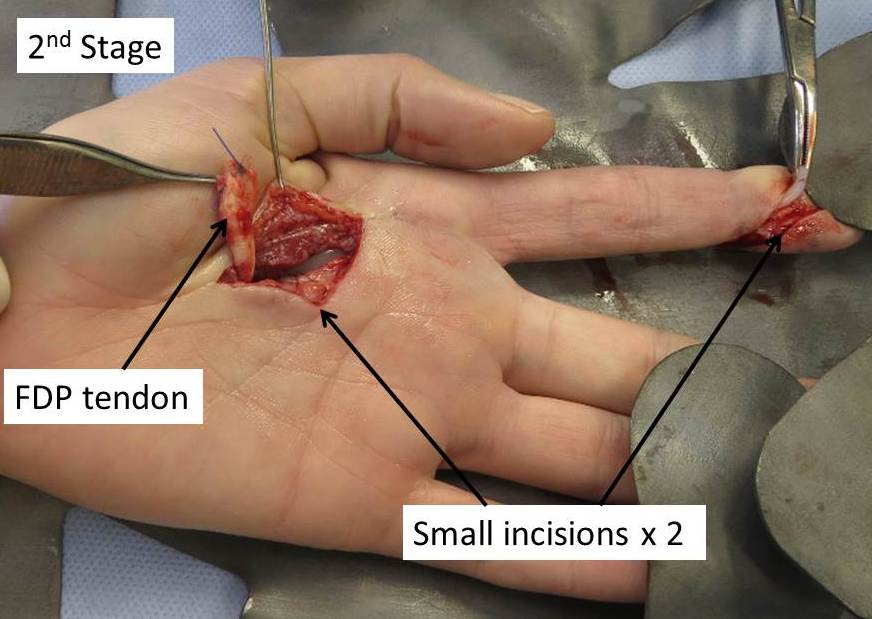
2nd Stage ( 8 - 12 weeks later)
- Once the finger has "settled" after the first surgery ie.
- Full range of motion
- Scar soft

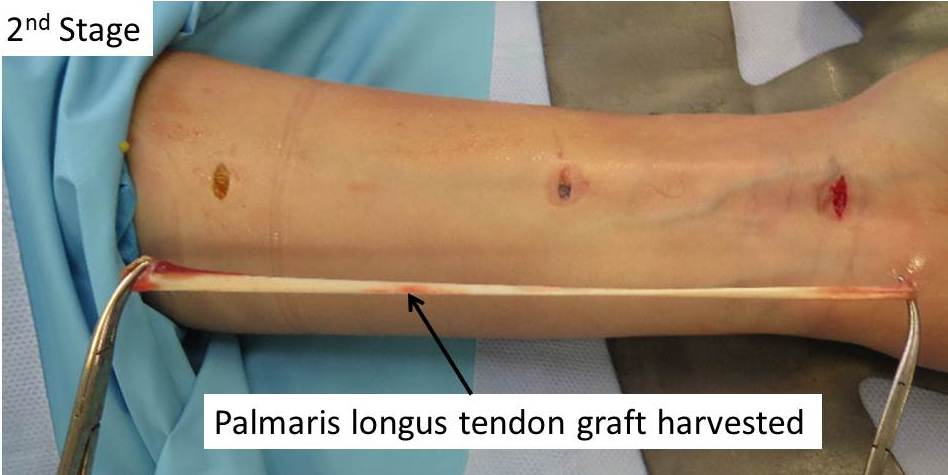
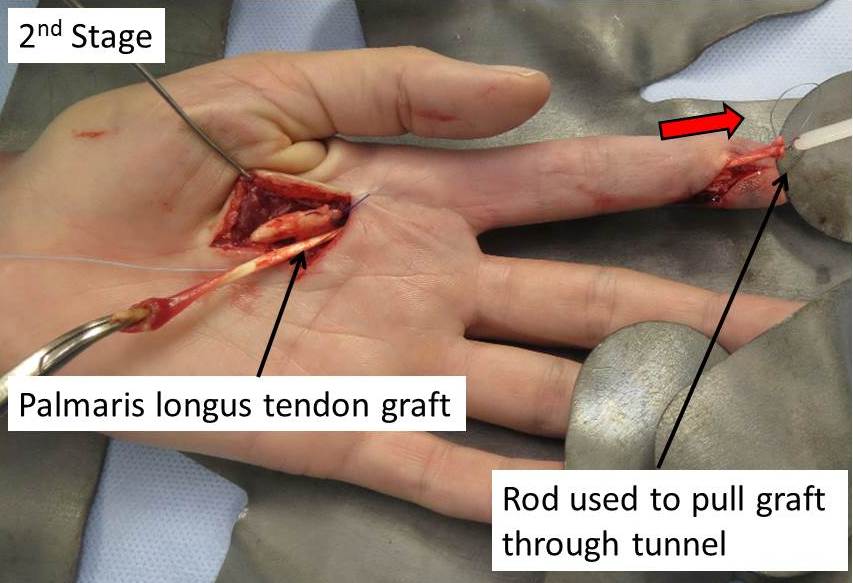
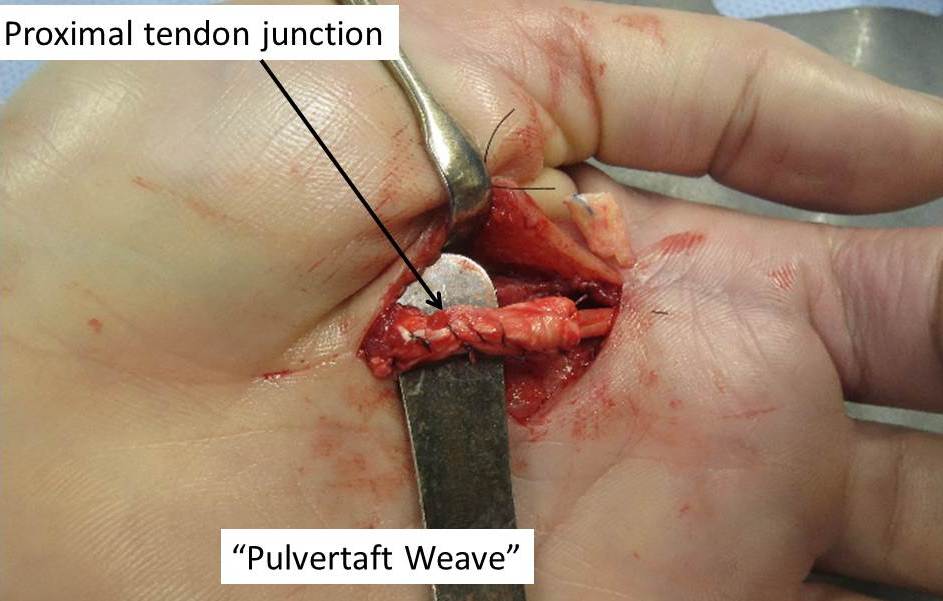
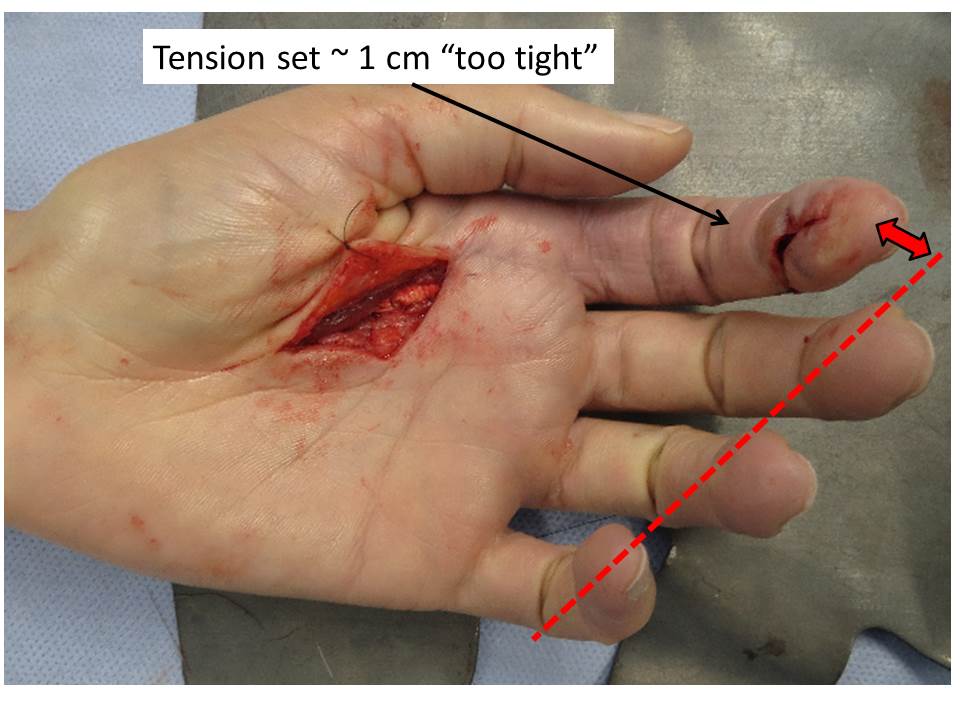
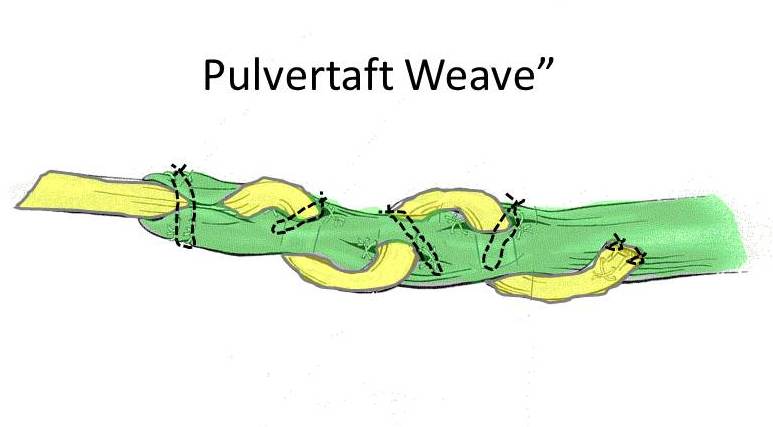
- At the second operation the plastic rod is removed and replacement with a tendon graft. The surgery is performed through much smaller incisions. The graft is usually harvested from the forearm ( Palmaris longus is a long thin tendon in the forearm which is present in ~ 85% of people; it serves no major function and is available for use elsewhere in the body)
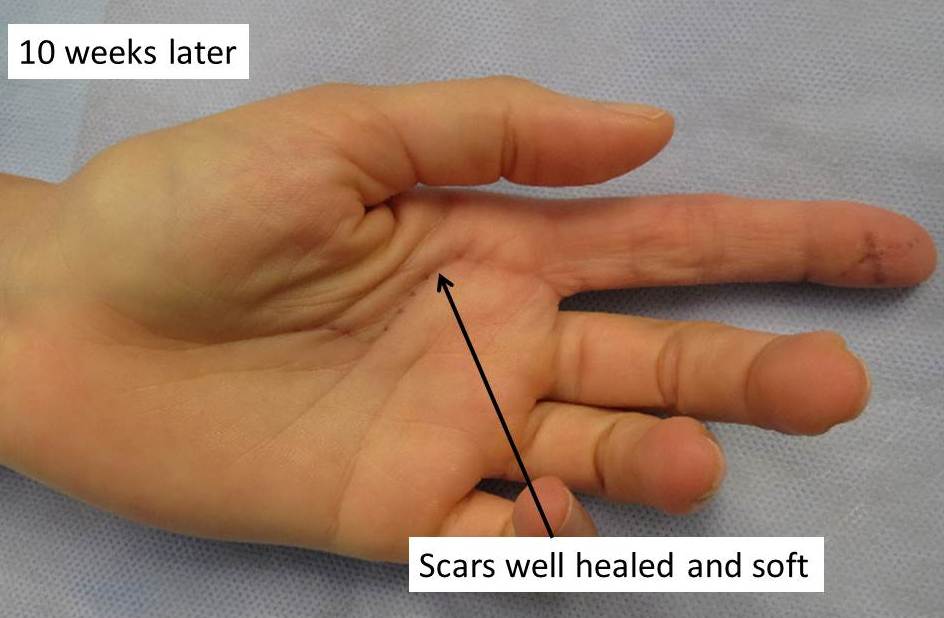
- The surgery is performed through Smaller incisions
- Plastic splint 6 weeks


- Significant activity restriction for 3 -4 months
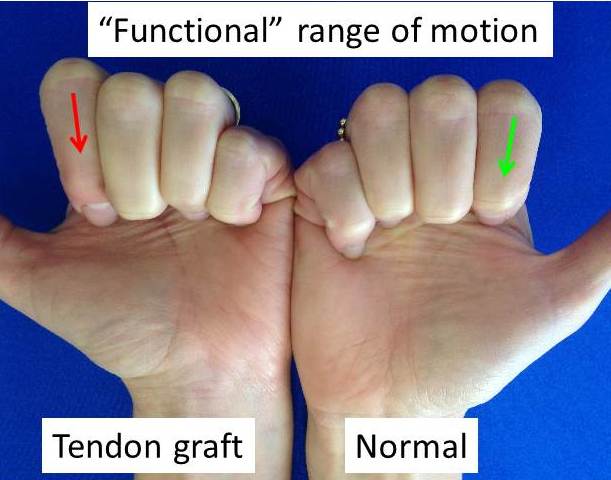
- Extensive Hand therapy but despite this there is often some restriction in range of motion at the end of the process.
LAST UPDATED ON 29/ 3 / 15